What Cranial Nerve Has Longest Subrachanoid Track
Description [edit | edit source]
The oculomotor nerve is the third cranial nerve (CNIII). It has somatic motor (general somatic efferent) and visceral motor (general visceral efferent-parasympathetic) functions.[1] Basically, the oculomotor nerve has three major functions which include[2]:
- Innervation of eye muscles for for gaze fixation and eye tracking (somatic motor)
- Innervation to the lens and pupil (autonomic parasympathetic)
- Innervation to the upper eyelid (somatic motor)
Root [edit | edit source]
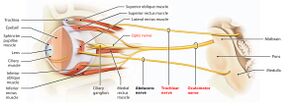
It originates from the oculomotor nucleus and the Edinger-Westphal nucleus within the midbrain of the brainstem. The oculomotor nerve exits the brainstem near midline at the base of the midbrain just caudal to the mammillary bodies. It passes through the cavernous sinus and proceeds through the supraorbital fissure to reach the orbit of the eye.[3]
Branches [edit | edit source]
The oculomotor nerve divides into superior and inferior branches in the anterior part of the cavernous sinus.
Superior branch innervates the superior rectus and the levator palpabrae superioris.
Inferior branch innervates the medial rectus, inferior rectus and inferior oblique.
[4]
Function [edit | edit source]
Motor [edit | edit source]
The oculomotor nerve is the chief motor nerve to the ocular and extraocular muscles. [1] The oculomotor nerves send somatic motor fibres to all extraocular muscles, except the superior oblique and lateral rectus. The superior branch supplies the superior rectus which elevates the eyeball, and the levator palpabrae superioris which raises the upper eyelid.
The inferior branch innervates the medial rectus which adducts the eyeball, the inferior rectus which depresses the eyeball and the inferior oblique which elevates, abducts and laterally rotates the eyeball. The superior oblique and the lateral rectus are supplied by the trochlear and abducens nerves respectively.
Parasympathetic [edit | edit source]
There are two primary functions of the autonomic parasympathetic (involuntary) oculomotor nerve. It constricts the pupil (miosis) by innervating the smooth muscle (sphincter pupillae) near the pupil. It also innervates the ciliary muscles.[3] The sphincter pupillae causes narrowing of the pupil in order to prevent diverging light rays from the corneal periphery creating a blurred image.[5] The ciliary muscle changes the shape of the lens during accommodation.
Sympathetic [edit | edit source]
The oculomotor nerve has no direct function, but sympathetic fibres run with the oculomotor nerve to innervate the superior tarsal muscle (helps to raise the eyelid).[6]
Clinical relevance [edit | edit source]
The oculomotor nerve can be susceptible to pathologies just like any nerve in the body. Usually, oculomotor nerve impairments may interfere with normal vision, which can irreversible or permanent.[2] Damage to the oculomotor nerve or any of its branches could lead to oculomotor motor nerve palsy (Third nerve palsy). Some of the causes include:
- Vascular ischemia
- Trauma
- Intracranial neoplasm
- Hemorrhage
- Congenital
- Idiopathic[7]
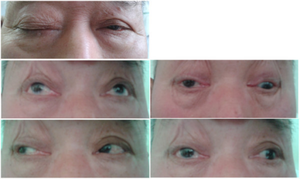
With unilateral third cranial nerve palsy (ie, oculomotor nerve palsy), the involved eye usually is deviated "down and out" (ie, infraducted and abducted), and there may be partial or complete ptosis. In addition, pupillary dilatation can cause anisocoria (greater in the light), symptomatic glare in bright light, and accommodation deficit that may cause blurred vision for near objects.[8] A complete third nerve palsy presents with ipsilateral mydriasis, bilateral ptosis, contralateral elevation deficit, and ipsilateral adduction and depression deficits.[9]
[10]
Assessment [edit | edit source]
Draw an 'H-shape' with a finger or the tip of a pen and ask the patient to follow your finger (or the pen) with their eyes. The head of the patient should be still during this process and the patient is asked to report any blurring of vision or double vision(diplopia). Total oculomotor nerve palsy implies involvement of all muscles innervated by the oculomotor nerve with pupillary involvement. There will be limitation of movements in all fields of gaze except abduction and intorsion. Incomplete palsy implies either partial limitation (paresis) of elevation, depression or abduction or even full movement in one or more of these directions.[11]
[12]
Treatment [edit | edit source]
Treatment initially involves medical management of systemic predisposing factors and conservative measures to obviate symptoms followed later by surgical intervention in non-resolving oculomotor nerve palsy.[11]
Mostly, in the acute phase, conservative management is usually considered. In case of the presence of diplopia, devices such as an eye patch, opaque contact lens, or a blurred lens to shield the eye affected may be useful interventions. [2] In other cases, Botulinum-toxin may be used in the correction of partial third nerve palsy with the component of adduction, especially when there is associated medial rectus involvement. In case there is a deficit in vertical deviation, prism glasses may be of help in correcting the abnormality.[2] [13]
Surgical management is usually warranted after six months of conservative management that yields no significant result. A strabismus surgery is carried out mostly to rectify this condition. The strabismus surgery fixes mal-alignment in extra-ocular muscles.[13]
Physiotherapy can be an effective treatment of choice after failed pharmacological treatment in patients with damage to cranial nerves III and VI.[14] Physiotherapy management of oculomotor nerve palsy include [[Neuromuscular Exercise Program |neuromuscular re-education]], kinesiotaping, laser therapy, trigger point therapy and electrical stimulation.
References [edit | edit source]
- ↑ 1.0 1.1 Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. 7th ed. Baltimore, MD: Lippincott Williams & Wilkins, 2014
- ↑ 2.0 2.1 2.2 2.3 Joyce C, Le PH, Peterson DC. Neuroanatomy, Cranial Nerve 3 (Oculomotor) [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537126/
- ↑ 3.0 3.1 Joyce C, Le PH, Peterson DC. Neuroanatomy, Cranial Nerve 3 (Oculomotor). Available from: https://www.ncbi.nlm.nih.gov/books/NBK537126. (accessed 4 May 2021)
- ↑ 3D4Medical From Elsevier. Anatomy Dissected: Cranial Nerve III (oculomotor nerve). Available from: http://www.youtube.com/watch?v=IfEnt4ulzb8 [last accessed 4/5/2021]
- ↑ Bloom J, Motlagh M, Czyz CN. Anatomy, Head and Neck, Eye Iris Sphincter Muscle. Available from:https://www.ncbi.nlm.nih.gov/books/NBK532252.(accessed 4 May 2021)
- ↑ Navin L. The Oculomotor Nerve (CN III). Available from:https://teachmeanatomy.info/head/cranial-nerves/oculomotor.(accessed 4 May 2021)
- ↑ Modi P, Arsiwalla T. Cranial Nerve III Palsy. Treasure Island (FL):StatPearls Publishing; 2018. Available from:https://europepmc.org/article/NBK/nbk526112.(accessed 4 May 2021)
- ↑ James G, Andrew GL. 2018. Third Nerve Palsy (Oculomotor Nerve Palsy) Treatment & Management. Available From: https://emedicine.medscape.com/article/1198462-treatment (accessed 4 May 2021)
- ↑ Grover SK. Revisiting Third Nerve Palsy. DJO. 2020; 31:18-22. DOI:http://dx.doi.org/10.7869/djo.561
- ↑ U-M Kellogg Eye Center in Ann Arbor. Third (3rd) Cranial Nerve Palsy. Available from: https://www.youtube.com/watch?v=AEL0xeJ_NSw https://www.youtube.com/watch?v=AEL0xeJ_NSw. [last accessed 4/5/2021]
- ↑ 11.0 11.1 Sadagopan KA, Wasserman BN. Managing the patient with oculomotor nerve palsy. Current opinion in ophthalmology. 2013;24(5):438-47.
- ↑ RegisteredNurseRN. Cranial Nerve Examination Nursing | Cranial Nerve Assessment I-XII (1-12) Available from: https://www.youtube.com/watch?v=oZGFrwogx14 [last accessed 4/5/2021]
- ↑ 13.0 13.1 Singh A, Bahuguna C, Nagpal R, Kumar B. Surgical management of third nerve palsy. Oman journal of ophthalmology. 2016 May;9(2):80.
- ↑ Rongies W, Bojakowski J, Koktysz L, Dolecki W, Lewinska AO, Krzeski A. Physiotherapy in Postinfection Injury to Cranial Nerves III, IV, and VI: A Case Study. American journal of physical medicine & rehabilitation. 2019; 98(6):e57-9. Doi: 10.1097/PHM.0000000000001060.
What Cranial Nerve Has Longest Subrachanoid Track
Source: https://www.physio-pedia.com/Oculomotor_Nerve